Delay in diagnosis, treatment significantly affecting those with endometriosis
Posted July 6, 2023 11:00 am.
Last Updated July 6, 2023 8:39 pm.
For years, Canadians with endometriosis, estimated to be one in 10, have been sounding the alarm over the long and painful journey to diagnosis and care and the many unknowns that come along with it.
Endometriosis causes tissue, similar to the lining of the uterus, to grow elsewhere in the body and it can grow all over the bowels, the bladder and the kidney system. The condition can lead to chronic pain, organ damage and infertility.
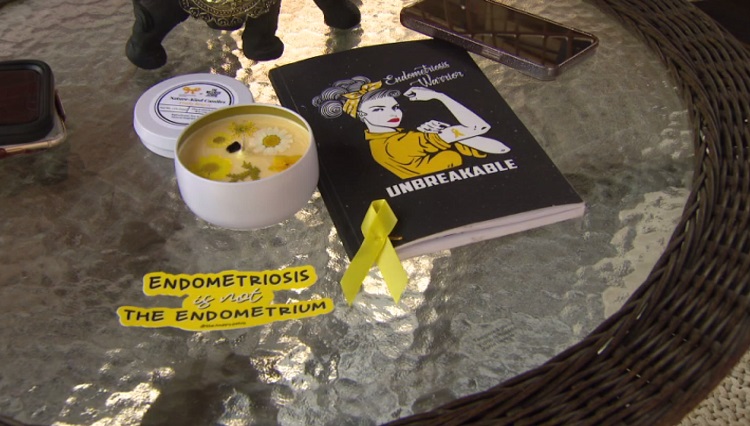
Those who suffer from the condition, who call themselves “endo-warriors”, are calling for more to be done to research endometriosis and provide resources for those who have been diagnosed.
Samantha Roberts struggled with her period since she was 12. She was put on birth control at age 13 or 14 by her doctor for the purposes of creating a lighter flow.
“Throughout my teenage years and going into my early 20s, I started realizing I had other symptoms that we couldn’t figure out what was wrong,” explained Roberts. “I had pain with sex; I was having trouble going to the bathroom without pain.”
She finally went to an OB-GYN and her initial assessment was that Roberts had endometriosis.
“Within a month of that appointment, I had my first surgery and that’s when I was diagnosed with endometriosis. And that would have been about three years ago.”
Surgery is required to diagnose endometriosis and further surgeries are often needed to remove the tissue or fibroids that grow as a result of the condition.
However, Roberts is still waiting for further treatment.
“I’ve only known for a short period of time that I’ve had endometriosis, but you know I’ve had symptoms for way longer, and then you know moving forward now … I am still getting more tests done.”
She said she had to wait over a year to see an endometriosis specialist at Women’s College Hospital after she was diagnosed and now, she is currently on a waitlist for a second surgery.
“And that could also take two to four years and I’m just living in the unknown right now.”
All she can do for now is just try and manage her pain.
“I do get really bad abdominal pain mainly on my right side. It affects my social life … there are days where I can’t get myself out of bed and it comes and goes,” said Roberts. “Some people think that your endo pain is only going to come when you’re on your period. But that’s not the case. It could be any day, all day.”
Roberts’ story is not unusual.
One of Canada’s leading experts for endometriosis, Dr. Sony Singh, who is also the Head of Obstetrics and Gynecology at The Ottawa Hospital, told CityNews it takes up to seven years for patients to get diagnosed.
“In my own practice when we did an audit, it took up to seven years for patients who first started to have symptoms, to finally have a diagnosis. We minimized the pain of understanding women’s health,” said Dr. Singh.
He said the pandemic also worsened wait times significantly, delaying diagnosis, care and especially surgeries. A delay in treatment can have horrific outcomes.
“For those patients that I deal with, their bowels can obstruct, they can lose a kidney. For some, there’s heavy menstrual bleeding as well. They’re dependent on IV iron. There’s a whole huge impact on their health … they can’t work. They can’t go to school. They can’t do what would make them an individual in society,” he added.
“You lose years of your life waiting for care, for diagnosis and surgery.”
Dr. Singh said a lack of resources and access to care continues to be an issue, even 17 years after he first started treating endometriosis patients.
While there has been an increase in the number of trained physicians, the demand is “massive.”
“We know that the disease is very common if we look inside every individual with a uterus and ovaries. The problem is that we aren’t going to do that, so we only end up seeing significant symptoms and we make a diagnosis. But it’s my feeling that it’s actually a huge societal issue that’s contributing to pain and infertility,” explained Dr. Singh.
He added the resources are just not available to treat everyone.
“First of all, is the clinic side to make the diagnosis with high-quality imaging and being able to see an expert we just don’t have the imaging capacity … The second access issue is surgery,” Dr. Singh said.
“After the pandemic hit, surgery was not prioritized … women’s health and the care of those with a uterus and ovaries was not up there. So, our backlog increased or delays in treatment increased.”
For Stacey Savary, it took seven to 10 years to receive her diagnosis. When she finally was able to have surgery, her endometriosis had progressed to Stage 4.
“In terms of treatment and care, you have to basically do your own research. When I say health plan of how you’re going to live with this kind of condition. And again, I wasn’t given any warning, no brochure, no pamphlet that this is going to be the rest of my life.”
Stacey said she believes it took so long to get diagnosed because her symptoms could look or show up like other things.
“If you have painful periods these days, basically that period is normal, like all women have painful periods, right? But if you have excessive bleeding and you’re passing out and you can’t be going to your normal day and you have to miss school or work. Those are key indicators that something else might be wrong, right?”
Dr. Singh tells CityNews there has been a push to make endometriosis a priority health issues through patient groups and federal action groups. As a priority health issue, there would be more funding and more attention. It also leads to the tracking of the condition.
“Data is everything when it comes to advocating for endometriosis care … once we get that information then we can actually understand where the problems lie,” said Dr. Singh.
The Public Health Agency of Canada tells CityNews it does not collect national surveillance data about endometriosis.
In a statement, the health agency said the government recognizes that endometriosis is a serious condition. However, the federal government’s primary role is supporting health care through funding while the province has jurisdiction over delivery of health care services.
They also add there is a Sexual and Reproductive Health Fund that was created in 2021 with an initial investment of $45 million and a further $36 million in 2023 to support a wide range of evidence-informed and innovative projects that address the pressing SRH needs of underserved communities in Canada.
Savary is encouraging other woman to advocate for help when they start to experience symptoms.
“Everything is digital and everything could be looked up and searched for, Googled,” said Savary. “At the same time if a young woman is feeling symptoms of endometriosis, that she could investigate further and get a proper, proper diagnosis. If someone doesn’t believe her, then go to another doctor and get a second opinion.”
Another reason why it’s important to diagnosed early is the effects the condition has on fertility. CityNews will be looking deeper into how endometriosis affects fertility in part two of this series.